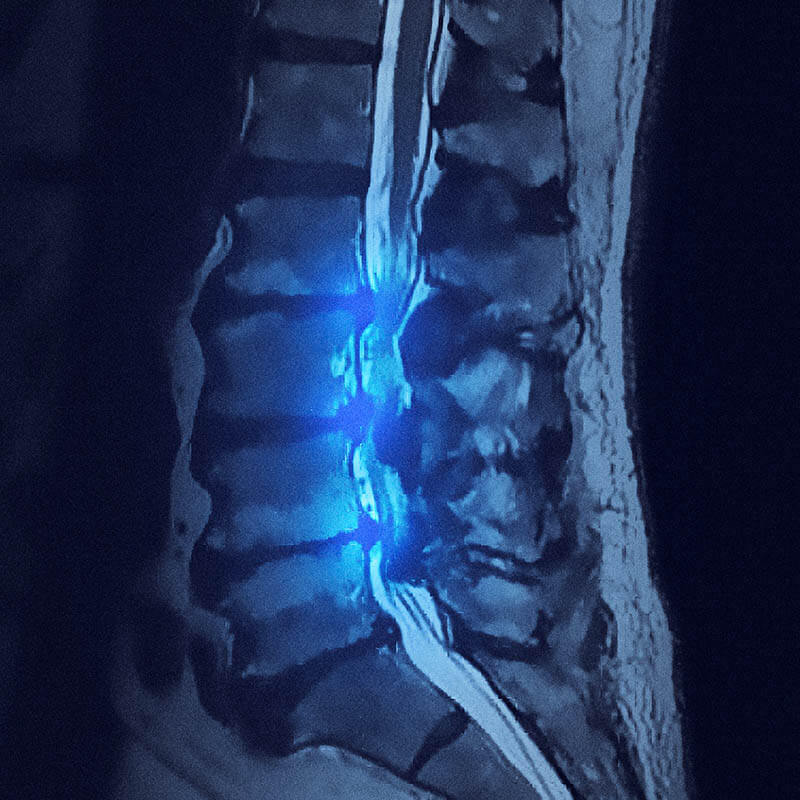
Comprehensive Diagnosis & Treatment of Spinal Stenosis
Lumbar spinal stenosis is the most common reason patients over the age of 65 undergo spine surgery. Most patients do not exhibit obvious symptoms of this condition caused by constriction of the spinal cord or spinal nerves. Individuals often discover they have spinal stenosis only when they experience generalized lower back pain and difficulty standing up straight.
Dr. Biscup utilizes state-of-the-art diagnostic tools to determine if spinal stenosis is responsible for your back pain. He explores non-invasive and surgical treatment options, creating a personalized treatment plan for you.
Conditions That May Cause Spinal Stenosis:
- Facet arthritis
- Degenerative disc disease
- Bone spurs
- Spondylolisthesis (slipped vertebra)
- Inflamed tissue
- Bulging discs
- Synovial cysts
- Degenerative scoliosis
Treatment Options
Dr. Biscup prefers to treat spinal stenosis with non-invasive techniques. If these treatments are ineffective, or if you suffer from a severe case of spinal stenosis, Biscup Spine will help you explore surgical treatment options.
There are three approaches to spinal stenosis treatment:
- Non-surgical treatments: In mild cases, non-prescription medicine and an exercise plan are enough to manage spinal stenosis. We may also suggest physical therapy as an additional non-surgical treatment option.
- Pain management treatments: We can help mitigate your pain while we work to resolve your stenosis. These treatments range from epidural injections (a procedure where medicine is placed directly into the spinal canal) to the use of radio waves that destroy painful nerve endings. Other treatments are available depending on the severity of your condition.
- Surgical treatments: Minimally invasive spinal decompression surgery is one of the most effective treatments for short- and long-term spinal stenosis relief. Other operations, such as spinal fusion, may be necessary if there is further instability of your spine.